Understanding Cataract Surgery
What is a cataract?
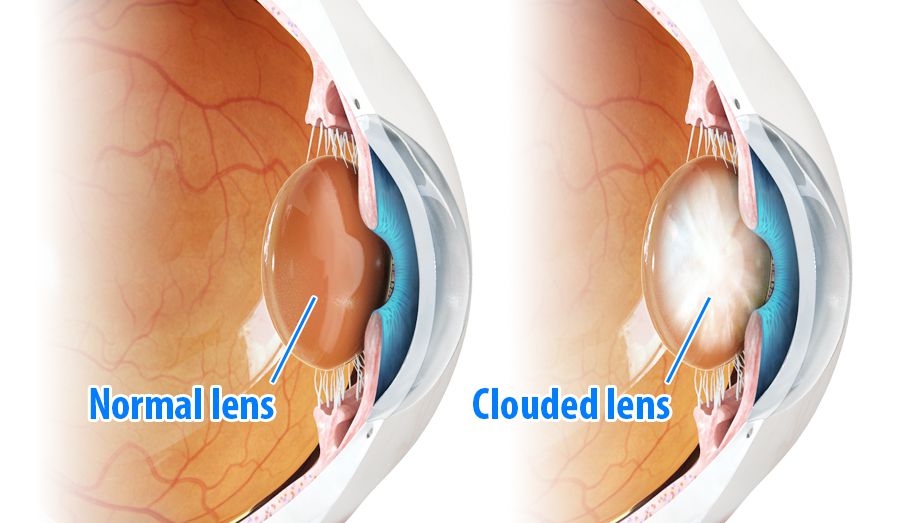
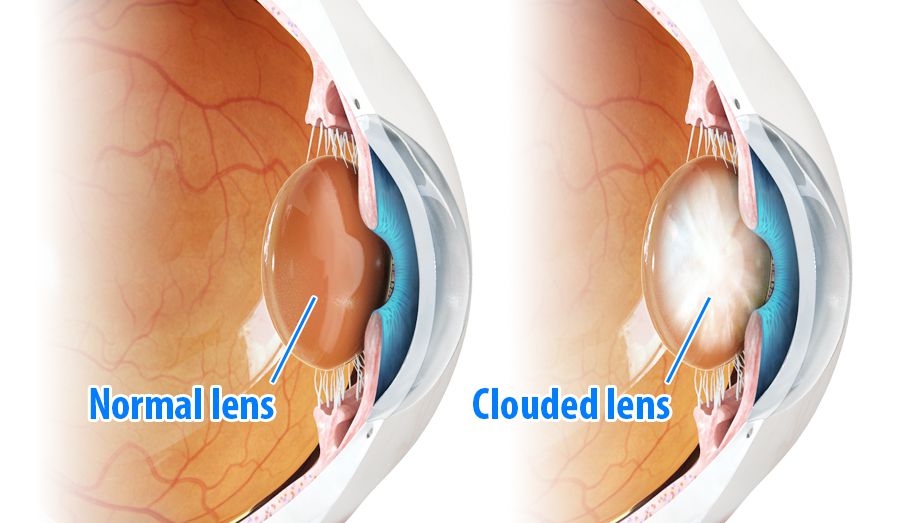
The natural lens of the eye is normally transparent. Cataract refers to a clouding or opacity of the natural lens of the eye. Surgery to remove cataract is the most commonly performed and possibly the most successful surgical procedure performed worldwide.
In order to understand how cataract affects the vision, it is helpful to understand the normal structure and function of the eye.
The eye can be compared to a camera. The pupil of the eye is like the aperture of a camera, regulating the amount of light entering the eye. Light is focussed by the cornea, the clear window into the eye, and the lens, which lies behind the pupil.
The retina is the light-sensitive nerve tissue that lines the inner wall of the eye, like the film in a camera. Rays of light enter the eye, passing through the cornea, pupil and lens before focusing on to the retina. The retina contains photoreceptors which convert light into electrical impulses. In the healthy eye these impulses are sent via the optic nerve to the brain, where sight is interpreted as clear, bright, colourful images.
The macula is a small area at the centre of the retina. It is very important as it is responsible for our central vision. It allows us to see fine detail for activities such as reading, recognising faces, watching television and driving. It also enables us to see colour.
If the lens of the eye becomes cloudy, this is known as a cataract, and if it is dense enough, it affects vision. The normal process of ageing causes cataract, however even young patients can develop cataract. Most people over the age of 60 years have some degree of cataract. An injury to the eye can cause a cataract as can the prolonged use of steroid medications for conditions such as asthma. Smoking, and some medical conditions such as diabetes increase the risk of cataract. Previous eye surgery such as vitrectomy (link) and other eye conditions may also cause a cataract to form.
It is impossible to predict how quickly a cataract will develop. In most people cataract formation occurs slowly over many years, but occasionally cataracts develop rapidly over a few weeks or months.
Cataracts are a little like a foggy lens in a camera. This foggy lens will obstruct the vision and decrease the clarity and brightness of objects that surround you. This can be very simply restored with a cataract operation.
Any or all of the following symptoms may occur as cataract develops:
- Deterioration in your vision. This may occur at far, near or both distances.
- Hazy or cloudy vision.
- Difficulty driving at night.
- Sensitivity to glare and light.
- Frequent changes to your glasses.
A cataract does not need be removed just because it is present. Surgery should only be considered when the cataract causes enough vision loss to interfere with daily activities such as work, driving, reading, hobbies, or watching TV. Surgery is performed when a person’s visual needs require it, and these needs vary between different people.
Leaving a cataract untreated does not damage the eye, but as the lens opacity worsens your vision will deteriorate until little sight remains. Surgery at this stage may be more difficult and carries a higher risk of complications.
If your optometrist has seen you and confirmed that you have cataracts, an initial consultation will take about half an hour. This involves a thorough history and examination to establish whether you actually need cataract surgery at this stage. The eye will be carefully examined with particular emphasis on the general health of the eye including the state of the retina. Biometric measurements of the eye will be taken with a laser (IOL Master 700 – link) to determine the precise power of the lens that will be needed to correct your sight.
There is no effective medical therapy for cataracts. Treatment involves a short surgical procedure to remove the cloudy lens and replace it with a tiny foldable lens implant that will take over the focussing of the eye.
Cataract surgery nowadays is almost always carried out as a day case procedure. In fact, most patients are only in the hospital for about two or three hours.
The surgery is performed in a hospital operating theatre. It is usually carried out using local anaesthetic eyedrops and mild sedation, though some patients may opt for general anaesthetic. Even patients who are rather anxious about the prospect of having eye surgery whilst awake usually cope very well once they understand what is involved and that the surgery itself is essentially painless.
Dr Isaacs performs cataract surgery on most patients using just local anaesthetic drops to numb the surface of the eye. This is known as topical anaesthesia. The benefits of this are that there is no risk to the eye from an injection of anaesthetic. Also, the vision recovers much more quickly after the procedure and the eye remains completely white afterwards.
The operation commences as soon as the eye is anaesthetized. A plastic drape is placed over the eye to keep the area of surgery as sterile as possible and also to catch the water that is continuously flowing around the eye during the procedure. The other eye is covered during the operation, and you will not be able to see details of the surgery, just the bright light of the operating microscope. A funnel with cool air flowing through it is placed on your chest to keep the drape off that part of your face. You will be asked to keep very still during the surgery, and simply to look up at the bright light of the microscope.
Modern cataract surgery has evolved tremendously over the last 20 years. The whole operation is performed through an opening of less than 3mm under the operating microscope. A tiny incision is made at the edge of the cornea, and the cataract is broken up inside the eye using an ultrasonic probe (phacoemulsification or phaco) before being removed from the eye.
After the cataract is removed, a tiny plastic folding lens is inserted into the capsular bag, the envelope that surrounds your natural lens. This part of the natural lens remains in the eye and supports the new plastic lens, or IOL. An eyepad and protective shield is placed over the eye overnight.
Typically the surgery itself takes around 10 minutes but the overall time in theatre is about 20 minutes.
After the operation you will return to the ward and usually have a cup of tea, as soon as you are ready you can go home. The eye may feel scratchy and slightly irritable for a couple of hours but normally settles within a day or two. Some patients require simple painkillers on the first night following surgery.
There are few restrictions on physical activity after your operation, but I advise against swimming for a week. You should however take it fairly easy for a few days. It is important not to rub the eye since the wound is self-sealing and there are no sutures. If you were to rub the eye vigorously then the would might leak. You won’t be able to drive until the vision has settled, no more than a day or so in most cases.
Eyedrops will be dispensed on the day of surgery. These should be used 4 times daily, started on the first day after surgery and continuing for 3 weeks postoperatively, until they are finished. If you have someone at home who can instil these for you, so much the better, but the nurses on the ward can demonstrate the technique if you are going to be on your own.
The exact timing of the drops does not matter, just spread them out fairly evenly during the day.
If you have been using drops for glaucoma, then restart these as usual the day after surgery.
Lubricating eye drops for dry eyes can be used any time as well.
Once the nurses are happy with your recovery you will be given a set of instructions and discharged from the surgery. You will be examined the next day in the clinic.
Until quite recently all patients who had cataract surgery had a standard lens implant that nearly always corrected vision for distance. This meant that the distance vision without glasses was nearly always excellent but patients struggled to read fine print.
In the last few years, lens implant technology has improved substantially and the number of options has increased. Hence the decision about which sort of lens to use is more complex. Options include monovision, where one eye is corrected for distance and the other for near. This strategy has been successfully used in contact lens patients for many years. However, it is not suitable for everyone.
Other options include multifocal lenses which correct for near and distance at the same time. These lenses can be extremely successful but they don’t suit everybody and can cause some optical side effects such as glare when driving at night.
Many patients have astigmatism (this is where the cornea, the clear window at the front of the eye is shaped more like a rugby ball than a soccer ball). Toric lens implants are designed to counteract the optical effects of astigmatism. They are very similar in appearance to a standard lens but are carefully rotated into a precise position during the surgery according to detailed calculations carried out beforehand.
Traditionally multifocal lenses were not suitable for anyone with significant astigmatism but even that has now been overcome with the arrival of multifocal toric lenses.
Dr Isaacs has experience with all these types of lenses and will help guide you towards an option that will maximise the visual success of your surgery.
After you have had your cataract procedure you will see much better at distance. Unless specified otherwise to you, you will most likely need only a pair of reading glasses to help you read.
In the majority of cases the recovery period after cataract surgery is short, and your vision will be much clearer the next day. In some patients it may take a few days for the vision to be restored.
Dr Isaacs will see you a few days after your operation to check the eye and find out how you are doing. At that point you will either be listed to have surgery to the fellow eye, or you will be discharged back to the care of your Optometrist.
Any surgical procedure carries risk. Using modern microsurgical techniques the risks of cataract surgery are low, however occasional complications can occur.
Haemorrhage and infection in the eye are extremely rare but potentially serious complications which may cause permanent loss of vision or even loss of the eye.
Retinal detachment may occur following cataract surgery and may require additional surgery.
Anaesthetic complications may occur. Local anaesthesia is usually given by eye drops so the risk is minimal. Unexpected movement of the eye during surgery can be potentially damaging to the eye. General anaesthesia always carries a very small but potentially severe risk. These risks will be explained by the anaesthetist prior to surgery.
If you have any questions concerning the procedure or possible complications please do not hesitate to contact Dr Isaacs or the team at Perth Retina for further explanation.